You'll receive the latest updates on new standards, guidelines, and educational resources, as well as expert insights to help enhance your laboratory's performance and compliance.
AST News Update January 2024: Sulbactam-Durlobactam: The “double beta-lactamase inhibitor” drug
Romney M. Humphries, Vanderbilt University Medical Center, Nashville, Tennessee, USA
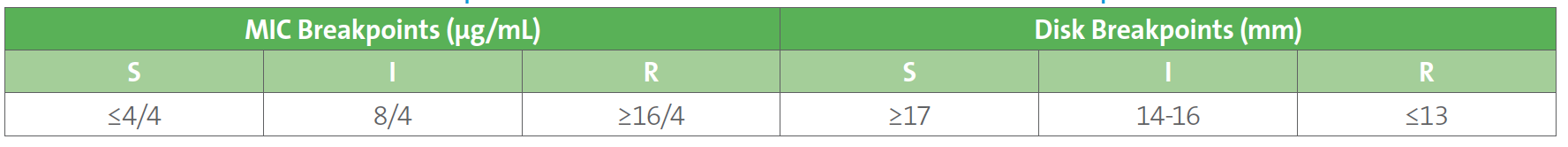
Many laboratorians are familiar with sulbactam, a β-lactamase inhibitor that is commercially combined with ampicillin, which was introduced in the US in 1986 to make ampicillin-sulbactam (“Unasyn”). Like many older β-lactamase inhibitors, sulbactam is itself a β-lactam, but has poor antimicrobial activity against most bacteria. Notably, sulbactam demonstrates bactericidal activity against Acinetobacter spp., due to sulbactam’s high affinity to penicillin-binding proteins expressed by Acinetobacter (PBP1 and PBP3), resulting in inhibition of bacterial cell wall synthesis and cell death.1 For decades, ampicillin-sulbactam has been used for its sulbactam component in the treatment of Acinetobacter spp. However, resistance to sulbactam has become common (45-80%) among contemporary Acinetobacter spp. isolates worldwide, in part due to the presence of Ambler class A, C, and D β-lactamases.2 Entasis Therapeutics, Inc. developed durlobactam, a non-β-lactam, diazabicyclooctane inhibitor of Ambler class A, C, and D β-lactamases expressed by Acinetobacter spp. The addition of durlobactam to sulbactam restores sulbactam’s activity against most Acinetobacter isolates. Sulbactam-durlobactam was approved by the United States Food and Drug Administration (FDA) in May 2023 for the treatment of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia caused by susceptible strains of Acinetobacter baumannii-calcoaceticus complex, in adults.3 The same breakpoints assigned by FDA were approved by CLSI in June 2023 (to be published in the 34th edition of CLSI M100 edition in February 2024), and are shown in Table 1. Resistance to sulbactam-durlobactam is rare as >97% of global isolates of A. baumannii-calcoaceticus complex show susceptibility to sulbactam-durlobactam. However, resistance has been shown with mutation to PBP3 or the presence of a metallo-β-lactamase such as NDM.4-6
The US FDA has cleared several testing options, including HardyDisk (Hardy Diagnostics), Oxoid Disc (Thermo Scientific), ETEST® (bioMérieux), and Sensititre 18-24 hour MIC (ThermoFisher Scientific). Not all tests are currently commercially available, now but are anticipated in early 2024.
Table 1. Sulbactam-Durlobactam Breakpoints for Acinetobacter baumannii-calcoaceticus Complex
References
1. Penwell WF, Shapiro AB, Giacobbe RA, et al. Molecular Mechanisms of Sulbactam Antibacterial Activity and Resistance Determinants in Acinetobacter baumannii. Antimicrob Agents Chemother. 2015; 59(3):1680-1689. Doi:10.1128/AAC.04808- 14; PMID:25561334; PMCID: PMC4325763.
2. Gales AC, Seifert H, Gur D, Castanheira M, Jones RN, Sader HS. Antimicrobial Susceptibility of Acinetobacter calcoaceticus- Acinetobacter baumannii Complex and Stenotrophomonas maltophilia Clinical Isolates: Results From the SENTRY Antimicrobial Surveillance Program (1997-2016). Open Forum Infect Dis. 2019 Mar 15;6(Suppl 1):S34-S46. Doi:10.1093/ofid/ofy293; PMID: 3085213; PMCID: PMC6419908.
3. Kaye KS, Shorr AF, Wunderink RG, et al. Efficacy and safety of sulbactam-durlobactam versus colistin for the treatment of patients with serious infections caused by Acinetobacter baumannii-calcoaceticus complex: a multicentre, randomised, active-controlled, phase 3, non-inferiority clinical trial (ATTACK). Lancet Infect Dis. 2023;23(9):1072-1084. Antimicrob Agents Chemother. 2020 64:e02534-19 doi: 10.1016/S1473-3099(23)00184-6. PMID: 37182534.
4. McLeod SM, Shapiro AB, Moussa SH, et al. Frequency and Mechanism of Spontaneous Resistance to Sulbactam Combined with the Novel β-Lactamase Inhibitor ETX2514 in Clinical Isolates of Acinetobacter baumannii. Antimicrob Agents Chemother. 2018. 62(2): e1576-17. doi: 10.1128/AAC.01576-17 PMID: 29133555; PMCID: PMC5786785.
5. Karlowsky JA, Lob SH, DeRyke CA, et al. In Vitro Activity of Ceftolozane-Tazobactam, Imipenem-Relebactam, Ceftazidime- Avibactam, and Comparators against Pseudomonas aeruginosa Isolates Collected in United States Hospitals According to Results from the SMART Surveillance Program, 2018 to 2020. Antimicrob Agents Chemother. 2022;66(5):e0018922. doi: 10.1128/aac.00189-22; PMID: 35491836; PMCID: PMC9112925.