You'll receive the latest updates on new standards, guidelines, and educational resources, as well as expert insights to help enhance your laboratory's performance and compliance.
What Labs Need to Know About the CDC’s Marburg Virus Advisory
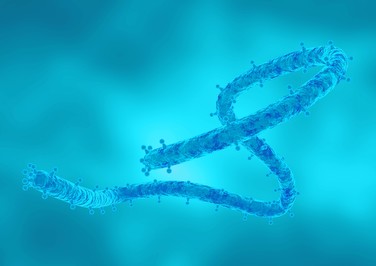
The Centers for Disease Control and Prevention (CDC) issued a Health Alert Network (HAN) Health Advisory on April 6 about two confirmed outbreaks of Marburg virus disease (MVD) in Equatorial Guinea and Tanzania. To date, no confirmed cases of MVD related to these outbreaks have been reported in the United States or other countries. The CDC Health Advisory summarizes their recommendations for case identification, testing, and clinical laboratory biosafety considerations in the United States.
MVD is a rare but highly fatal viral hemorrhagic fever. A person with MVD is not contagious until symptoms appear. Symptoms may include fever, headache, muscle and joint pain, fatigue, loss of appetite, gastrointestinal symptoms, or unexplained bleeding. Marburg virus is spread through contact(through broken skin or mucous membranes) with the blood or other body fluids of a person who is sick with or has died from MVD, with the body fluids of infected animals, or with needles or other fomites that are contaminated with the virus. Marburg virus is not airborne.
There is currently no Food and Drug Administration (FDA)-approved vaccine or treatment for MVD. In the absence of early diagnosis and appropriate supportive care, MVD has a high mortality rate of 23%–90%. With early intensive supportive care and fluid replacement, mortality rates may be lower.
According to CDC, clinical laboratories can safely perform common diagnostic testing for patients with suspected MVD by following Standard Precautions for All Patient Care and Universal Precautions for Preventing Transmission of Bloodborne Infections.
Under the Occupational Safety and Health Administration’s (OSHA’s) Bloodborne Pathogens Standard, laboratories handling blood and body fluids must have a written Exposure Control Plan in place to eliminate or minimize employees’ risk of exposure to blood or other potentially infectious materials. Proper PPE should be available and staff should be trained to properly don and doff their PPE. If a facility does not have the appropriate risk mitigation capabilities, the specimen should be forwarded to another facility that does.
For more guidance on the collection, transportation, and submission of specimens, visit the CDC website here.