You'll receive the latest updates on new standards, guidelines, and educational resources, as well as expert insights to help enhance your laboratory's performance and compliance.
Changes in Methodology and Breakpoints for Staphylococcus spp. Linezolid and Tedizolid Disk Diffusion Tests
Robert Bowden, Beth Israel Deaconess Medical Center, Boston, MA
Andrea Ferrell, BD Life Sciences, Sparks, MD
Robert Bowden, Beth Israel Deaconess Medical Center, Boston, MA
Andrea Ferrell, BD Life Sciences, Sparks, MD
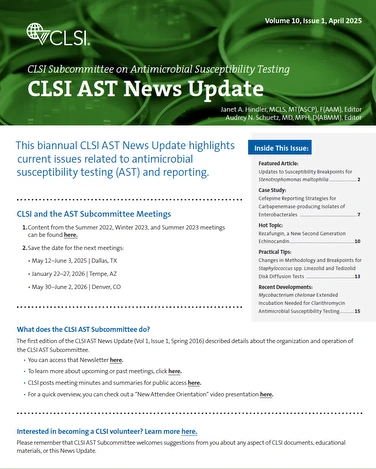
CLSI AST News Update | Volume 10, Issue 1, April 2025
Tedizolid disk diffusion breakpoints for staphylococci, beta-hemolytic streptococci and viridans streptococci were added to CLSI M100 in 2024. In addition, as related to disk diffusion testing, changes were made to oxazolidinone quality control ranges, linezolid breakpoints, and zone measurement guidance for Staphylococcus spp. using reflected light as shown in Table 11 and Figure 1.


How did these revisions and additions for oxazolidinones and staphylococci come about?
Following the introduction of tedizolid MIC breakpoints to CLSI M100 in 2016, the Methods Development and Standardization Working Group of CLSI’s AST Subcommittee began work to establish tedizolid disk diffusion quality control ranges and zone diameter breakpoints. This revealed issues with previous zone diameter breakpoints for testing staphylococci with linezolid, which was used as an in-class control agent for testing tedizolid. In addition, Staphylococcus aureus ATCC® 25923 yielded a higher number of reproducible results for both linezolid and tedizolid when zones were measured with reflected light as opposed to transmitted light. Reading with transmitted light had been the previous CLSI recommendation.3
Why was transmitted light previously used for testing linezolid with staphylococci?
Oxazolidinone resistance remains uncommon among staphylococci. Because resistant isolates were rarely encountered when CLSI linezolid MIC and disk diffusion breakpoints were first established in 2006, only a susceptible breakpoint was assigned (≤4 μg/mL and ≥21 mm Susceptible). Disk diffusion zones were initially measured using reflected light.4 However, a 2007 publication reported that among a small set of non-susceptible isolates (n=15) submitted to the Centers for Disease Control and Prevention (CDC), 53.3% were incorrectly categorized as susceptible when tested by disk diffusion. However, these errors were reduced by measuring zones using transmitted light that better detected faint or pinpoint growth within the zones of inhibition.5 Subsequently, in 2008 a comment was added to CLSI M100 Table 2C stating that, “when testing linezolid, disk diffusion zones should be examined using transmitted light. Organisms with non-susceptible results should be confirmed using an MIC method.” In 2010, resistant breakpoints of ≥8 μg/ mL and ≤20 mm were established.6 However, an evaluation of linezolid resistance-enriched datasets by CLSI in the past few years demonstrated that the zone diameter breakpoints were still resulting in a >15% very major error rate for S. aureus, despite use of transmitted light.
What impact do these changes have?
While MIC breakpoints for linezolid remain ≤4 μg/mL “S” and ≥8 ug/mL “R” with no intermediate MIC interpretive category, the introduction of an intermediate category for disk diffusion only and revision of the “S” and “R” zone diameter breakpoints have significantly improved the accuracy of disk diffusion results as compared to MIC testing by reducing the number of very major errors to ≤1.5%.
Use of reflected light when reading Staphylococcus spp. zone diameters harmonizes with the methodology used for enterococci when testing linezolid and when reading results for all other antimicrobial agents, simplifying the reading process and reducing the likelihood that methodological errors will occur.
Lastly, disk breakpoints for tedizolid have been established for the first time, enabling many more laboratories to perform tedizolid testing in-house, decreasing laboratory costs and improving turnaround time.
References
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 34th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2024.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 18th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2008.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 16th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2006.
- Tenover FC, Williams PP, Stocker S, Thompson A, Clark LA, Limbago B, Carey RB, Poppe SM, Shinabarger D, McGowan JE Jr. Accuracy of six antimicrobial susceptibility methods for testing linezolid against staphylococci and enterococci. J Clin Microbiol. 2007 Sep;45(9):2917-22. doi: 10.1128/JCM.00913-07. Epub 2007 Jul 18. PMID: 17634301; PMCID: PMC2045282.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 20th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2010.